Lymphedema
Here we explain symptoms, diagnosis and causes of lymphedema.
What is Lymphedema?
Damage to the lymphatic vessel system disturbs the capacity to transport waste. Protein and tissue fluid can no longer be carried away and instead accumulate in interstitial tissue, this causes the tissue to swell, so-called lymphedema. The latter always manifests itself in that part of the body where lymph draining ability is impaired. Especially affected are arms and legs. Lymphedema can also occur on organs, the head or genitals. It afflicts women more frequently than men.
Depending on the cause, a distinction is made between primary and secondary lymphedema.
Primary Lymphedema
Lymphedema is described as “primary” when already at birth a malformation of the lymphatic vessels exists. Possible causes of primary lymphedema could be:
- Complete absence of lymphatic vessels, usually in individual parts of the body (aplasia/atresia)
- Lymphatic vessels are too narrow or too few (hypoplasia)
- Distended vessels (hyperplasia, lymphangiectasis)
- Hardening of lymph nodes (lymph node fibrosis)
- Absence of lymph nodes (lymph node agenesia)

Compliance is excremly important treating lymphedema.
Primary lymphedema tends to develop between puberty and the age of 35. However, it can already be present at birth or develop after the age of 35. Primary lymphedema can be hereditary but usually occurs sporadically.
Secondary Lymphedema
One speaks of “secondary lymphedema” when damage to the lymph function was sustained through external causes. It is then the result of damage to the lymph vessels or lymph nodes. The causes of secondary lymphedema are:
- Injury
- malignant disease (eg a tumour)
- Inflammation of the skin (eg erysipelas)
- Parasites
- Operations and/or radiation
The principal cause of secondary lymphedema in western industrial nations are operations for cancer in which lymph nodes are partially or completely removed as well as radiation treatment.
Lymphedemas differ in appearance, site of the disease and shape. Unfortunately lymphedema is often diagnosed too late. Many afflicated persons are not receiving appropriate treatment and consequently the number of patients in Germany is according to the German Society for Vascular Disease (Deutsche Gefäßliga) estimated to be approx 80,000.

Image of lymphoedema.
Diagnosis
Lymphedema can usually be quickly diagnosed on the basis of a detailed anamnesis and a clinical examination (inspection, palpation). Indications of lymphedema the consulting physician should heed are:
- Skin colour is discoloured normal to light brown-grey
- Tissue consistency is increased
- Deep skin folds
- In the early stages of edema skin indents when pressed and holds the indentation. This is no longer possible in the later stages
- It is not possible to lift a skin fold from over the dorsum of the foot or fingers. Important: is this not possible, this is still not a clear indication that lymphedema exists.

On the right you can see the Stemmer’s sign.
Stages of Lymphedema
Lymphedema does not occur overnight but develops insidiously. However, once edematization has begun, the process will continue if left untreated. This is amongst other things connected with the fact that the skin´s defence function deteriorates because of lymphedema. Bacterial skin infections, such as eg erysipelas can develop, which in turn affect the lymphatic vessels. The edema worsens.
There are different degrees of severity relating to lymphedema. The severity depends on the stored amount of lymph fluid in the tissue. In the early stages the swollen skin area still clearly indents when pressed with the thumb. If the indentation does not disappear immediately again, this indicates edema. In more advanced stages the swelling has developed to such an extent that the extremities appear totally deformed. This condition leads to a worse defence function of the skin. That is why lymphedema tends to lead in more advanced stages to bacterial skin infections, such as erysipelas. These infections in turn affect the lymphatic vessel system and thus worsen lymphedema.
The development of lymphedema can be divided into the following four stages:
Stage 0: Latent Edema
The lymphatic vessel system has already sustained damage and already functions on a reduced level. It can still however make up for lymph drainage conditions. Edema is not (yet) present.
Stage I: Reversible Edema
The lymphatic vessel system can´t cope. Soft tissue swelling occurs mainly in the evening. The swelling can be fully reversed overnight or after a few days with limb elevation.
Stage II: Chronic irreversible Edema
The swelling has clearly hardened. The skin no longer indents when pressed and the edema cannot be reversed after longer periods of rest.
Stage III: Elephantiasis
The swelling takes on extreme dimensions. The leg is badly deformed. The skin is hard and characterized by wart-like outgrowths. Due to the development of lymph sacks and excessive bulging there is increased danger of erysipelas.
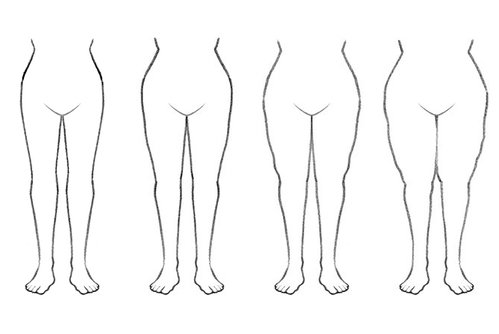
The different stages of lymphoedema.





